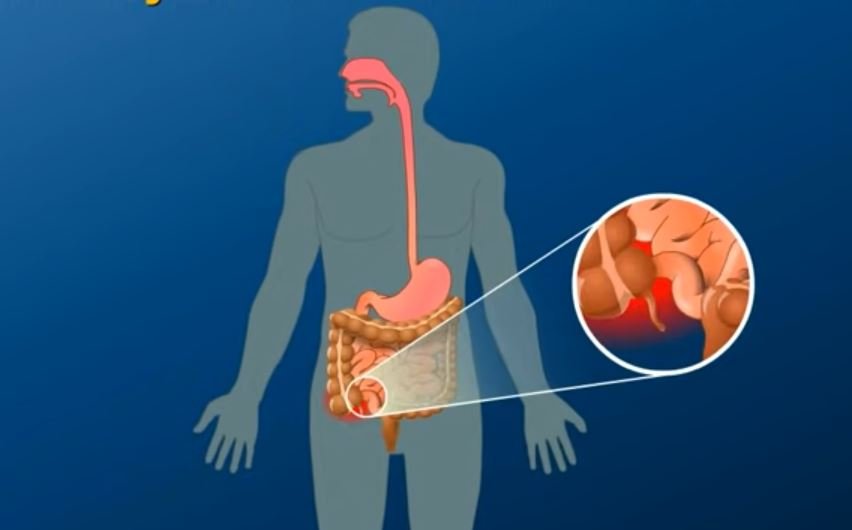
Millions of people worldwide suffer from Inflammatory Bowel Disease (IBD), a complicated, chronic illness that goes beyond a simple stomachache. IBD, which is characterized by ongoing inflammation of the digestive tract, can be erratic, with painful flare-ups interspersed with periods of remission. However, with improvements in research and treatment, there is increasing hope that people with IBD can live happy, healthy lives.
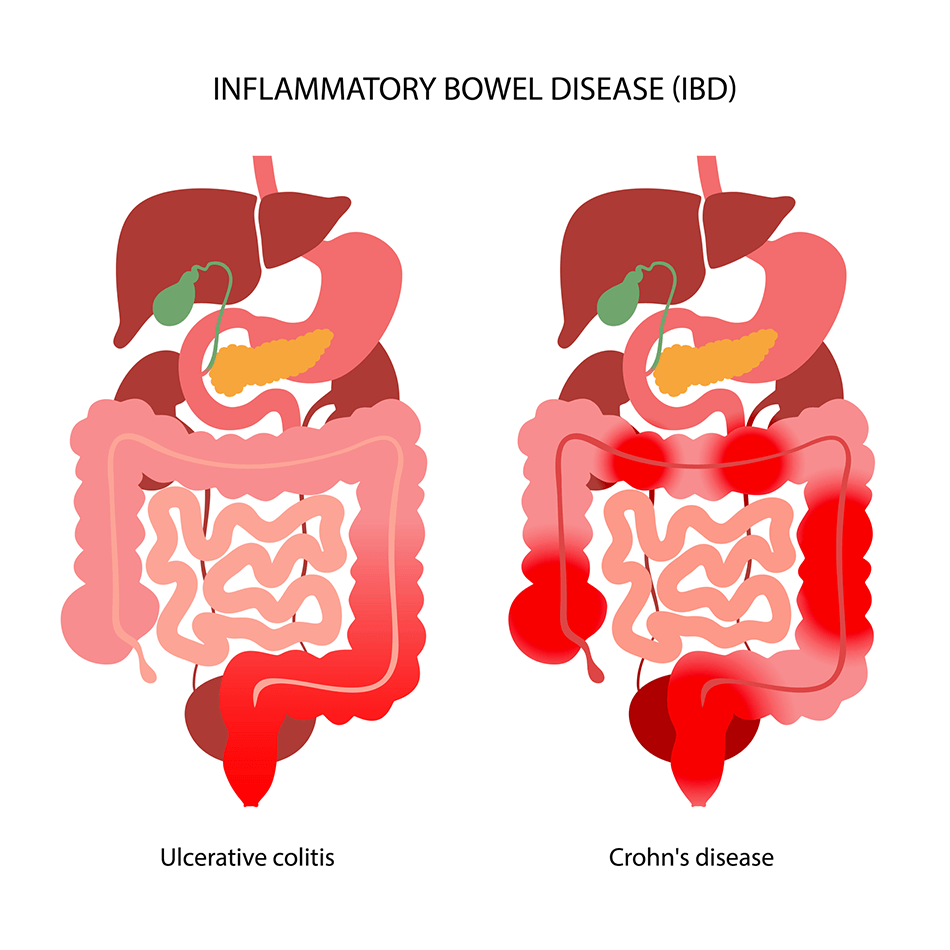
Crohn’s disease and ulcerative colitis are the two main conditions that are included under the general term IBD. Although they both induce gastrointestinal (GI) tract inflammation, their effects are different. Ulcerative colitis mainly affects the colon and rectum, whereas Crohn’s disease can affect any part of the digestive system. Effective management requires knowledge of their variations, triggers, and available treatments.
Key Facts About Inflammatory Bowel Disease (IBD)
| Category | Details |
|---|---|
| Types of IBD | Crohn’s Disease, Ulcerative Colitis |
| Common Symptoms | Diarrhea, abdominal pain, weight loss, rectal bleeding, fatigue |
| Causes | Autoimmune response, genetic predisposition, environmental factors |
| Risk Factors | Family history, smoking, diet, gut microbiome imbalances |
| Treatment Options | Medication, lifestyle changes, surgery |
| Estimated Cases (US) | 1.6 million people |
| Most Affected Age Group | 15 to 35 years old |
| Potential Complications | Colon cancer, bowel perforation, toxic megacolon |
Dissecting IBD: Ulcerative Colitis vs. Crohn’s
Although ulcerative colitis and Crohn’s disease are similar, they have different physiological effects.
- Crohn’s disease: Usually affecting the deeper layers of the digestive tract, it can develop anywhere from the mouth to the anus. Serious complications may result from strictures (intestinal narrowing) and fistulas (abnormal connections between organs).
- Ulcerative Colitis: Causes persistent inflammation and ulcers, primarily affecting the colon and rectum. It typically only affects the intestine’s innermost lining, in contrast to Crohn’s.
To reduce symptoms and avoid long-term issues, both conditions need to be continuously managed.
What Causes IBD?
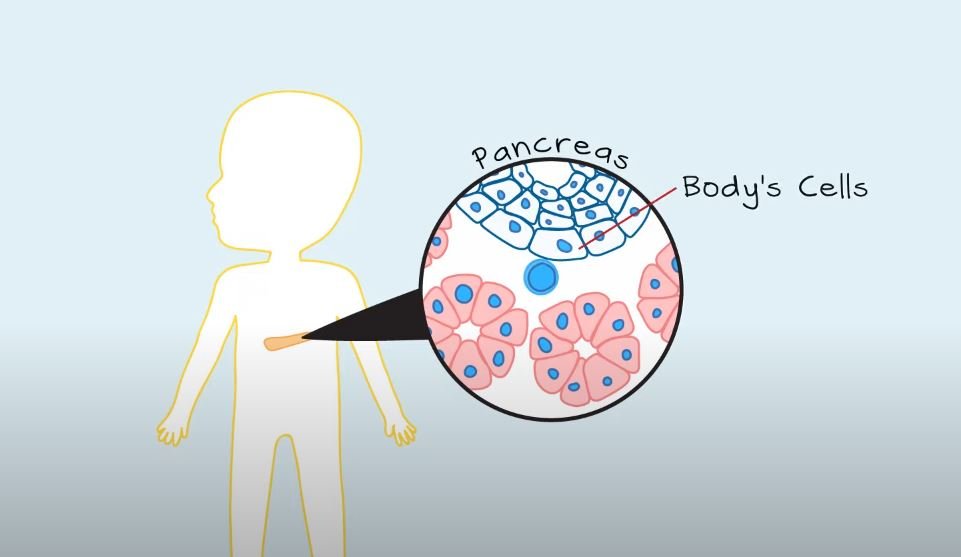
Although the precise cause of IBD is still unknown, scientists think a combination of immune, environmental, and genetic factors play a role.
- Genetics: Up to 20% of people with IBD have a family member who also has the condition.
- Immune System Dysfunction: The GI tract’s healthy cells are mistakenly attacked by an overactive immune system.
- Environmental Triggers: Unbalanced gut flora, stress, smoking, and diet can all contribute to symptom flare-ups.
IBD cannot be avoided, but its effects can be greatly lessened with early intervention and lifestyle changes.
Recognizing Symptoms: When to Seek Help
Symptoms of IBD can be mild, severe, or somewhere in between, with flare-ups that come and go. Some of the most common signs include:
✔ Chronic diarrhea
✔ Abdominal pain and cramping
✔ Unintentional weight loss
✔ Rectal bleeding
✔ Extreme fatigue
✔ Loss of appetite
If symptoms persist for several weeks, a consultation with a gastroenterologist is recommended.
How Is IBD Diagnosed?
Diagnosing IBD involves a combination of medical history, lab tests, and imaging. Physicians often use the following tests:
- Blood tests (to check for anemia and inflammation)
- Stool samples (to rule out infections)
- Colonoscopy (to inspect the colon and take biopsies)
- CT/MRI scans (to detect complications)
- Capsule endoscopy (to examine the small intestine)
Since IBD shares symptoms with other digestive disorders like Irritable Bowel Syndrome (IBS), precise diagnosis is critical for effective treatment.
Treatment Strategies: A Holistic Approach
Managing IBD requires a tailored, multi-faceted approach that includes medications, dietary changes, and, in severe cases, surgery.
1. Medications for IBD
Doctors may prescribe a range of medications to control inflammation and prevent damage:
- Anti-inflammatory drugs: Corticosteroids and aminosalicylates help reduce gut inflammation.
- Immunosuppressants: These drugs, such as azathioprine, weaken the immune response.
- Biologic therapies: Targeted treatments like anti-TNF drugs (e.g., infliximab) block inflammatory proteins.
- Antibiotics: Often used to treat infections resulting from fistulas or abscesses.
2. Diet and Lifestyle Modifications
While no specific diet cures IBD, some foods can trigger flare-ups. Here are recommended dietary changes:
✔ Eat smaller, frequent meals to ease digestion.
✔ Choose low-fiber foods during flare-ups.
✔ Limit dairy if lactose intolerant.
✔ Avoid processed foods and artificial additives.
✔ Stay hydrated to prevent dehydration from diarrhea.
Additionally, managing stress, maintaining a healthy sleep cycle, and regular exercise can improve overall well-being.
3. Surgical Interventions
For severe cases, surgery may be required when medication fails. Common procedures include:
- Colectomy: Removal of the colon, often for ulcerative colitis patients.
- Bowel resection: Removing damaged portions of the intestine in Crohn’s disease.
- Ostomy surgery: Redirecting waste through an opening in the abdomen if necessary.
Surgical treatments have significantly improved outcomes, with many patients experiencing long-term relief.
IBD Complications: What You Should Know
If left untreated, IBD can lead to severe complications, including:
✔ Colon cancer – Long-term ulcerative colitis increases the risk.
✔ Toxic megacolon – A potentially life-threatening condition requiring urgent care.
✔ Bowel perforation – Can lead to dangerous infections.
✔ Nutrient deficiencies – Due to malabsorption.
Other long-term complications include osteoporosis, kidney stones, anemia, and joint pain. Regular medical monitoring is essential to catch these issues early.
Using Innovation to Manage IBD
Thanks to proactive lifestyle changes, early diagnosis, and medical advancements, IBD is becoming more manageable even though it is a lifelong condition. Millions of people are given hope by the personalized therapies and possible future cures that researchers are still creating.
IBD patients can flourish with the right care, a solid support network, and medical direction. The secret to success, whether it’s through medicine, surgery, or dietary adjustments, is to remain informed, take initiative, and keep a resilient outlook.