Hunter’s disease, also referred to as Mucopolysaccharidosis Type II (MPS II), is a very uncommon genetic condition that subtly but persistently affects almost all of the body’s organ systems. It is a condition that frequently goes undiagnosed until symptoms worsen, leaving families in a state of confusion.
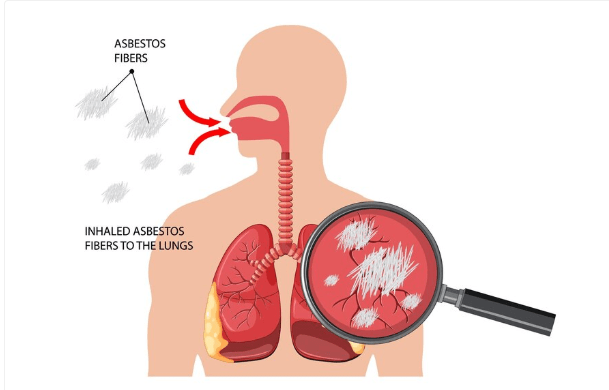
This disorder causes a toxic accumulation of glycosaminoglycans (GAGs), which over time damages tissues and organs by interfering with the body’s ability to break down complex sugars. This accumulation makes it one of the most complicated hereditary diseases that science has identified, leading to progressive complications such as heart disease, skeletal abnormalities, and cognitive decline.
Hunter’s Disease: Key Facts and Figures
| Category | Details |
|---|---|
| Medical Name | Mucopolysaccharidosis Type II (MPS II) |
| Cause | Deficiency of iduronate-2-sulfatase enzyme |
| Inheritance Pattern | X-linked recessive disorder (primarily affects males) |
| Common Symptoms | Enlarged facial features, stiff joints, breathing difficulties |
| Cognitive Impact | Possible intellectual disabilities in severe cases |
| Typical Prognosis | Life expectancy varies; severe cases may lead to early death |
| Current Treatments | Enzyme replacement therapy (Elaprase), symptom management |
| Ongoing Research | Gene therapy trials exploring long-term solutions |
The Science Behind Hunter’s Disease
Hunter’s disease is fundamentally caused by a single genetic error. Iduronate-2-sulfatase is a vital enzyme that the body cannot produce in sufficient amounts when the IDS gene is mutated. In cells, this enzyme is essential for the breakdown and recycling of specific sugar molecules. Without it, the body’s capacity to function normally is gradually overwhelmed by these sugars, which start to build up like waste in a clogged drain.
The disease is nearly exclusively found in males due to its X-linked recessive nature. Because they have a second functional X chromosome, female carriers usually do not experience symptoms. However, the effects are severe for males who are affected; symptoms start to show up in early childhood and get worse over time.
How Hunter’s Disease Transforms the Body
Hunter’s disease does not occur suddenly. Rather, as GAG accumulation rises, it affects various body parts in a gradual and progressive manner.
Children with Hunter’s disease can be identified from their peers by their thickened skin, large head, and coarse facial features, which are the most obvious early symptoms. More worrisome symptoms, such as limited joint mobility, respiratory problems, hearing loss, and an enlarged liver and spleen, appear as the disease progresses.
The neurological system is also impacted in extreme situations. Some kids develop severe intellectual disabilities as a result of losing developed abilities like speech and coordination. Walking and daily activities become challenging as the body grows weaker due to stiffening joints, weakening muscles, and thickening bones.
Why Diagnosing Hunter’s Disease is a Race Against Time
Hunter’s disease is frequently misdiagnosed despite its devastating effects. Early symptoms like breathing problems, recurrent infections, and developmental delays are easily confused with other illnesses, which delays necessary treatment.
The most reliable method of diagnosing the condition is still genetic testing. The disease can be confirmed by a straightforward blood test that looks for iduronate-2-sulfatase deficiencies. Furthermore, MRI scans reveal information about skeletal and neurological damage, and urine tests can detect elevated glycosaminoglycan levels.
Early detection is essential. The likelihood of slowing the progression of the disease and enhancing quality of life increases with the timing of treatment.
A Future Without Hunter’s Disease? Gene Therapy’s Potential
There was no proven cure for Hunter’s disease for many years. Physicians were limited to treating patients’ symptoms and offering supportive care. But that story has changed as medical science has advanced.
Enzyme replacement therapy (ERT) provides patients with a lifeline today. Some of the effects of the disease are lessened by ERT, which helps lower the accumulation of dangerous sugars by introducing the missing enzyme into the bloodstream. The catch is that ERT cannot stop neurological decline in extreme cases because it does not penetrate the blood-brain barrier.
Here’s where gene therapy is starting to change the game. Researchers are looking into ways to give patients’ cells functional copies of the IDS gene so they can make the missing enzyme on their own. Promising results from early clinical trials indicate that some patients who received experimental treatments were able to maintain stable enzyme levels for prolonged periods of time.
Making sure the medication gets to the brain is the largest obstacle. Gene therapy has the potential to change Hunter’s disease from a fatal illness to one that can be controlled if researchers can get past this obstacle.
The Hidden Cost of Hunter’s Disease: The Emotional and Financial Struggles
Hunter’s disease has a significant emotional and financial impact on families in addition to its physical effects. Enzyme replacement therapy alone can cost over $500,000 annually, making it one of the priciest medical procedures available today.
The emotional toll is equally as great. Knowing that current treatments can only postpone the inevitable, parents must watch as their children gradually lose the abilities they once possessed. When there seems to be no hope, many turn to advocacy groups, support groups, and medical trials.
How You Can Help Advance Research and Awareness
Hunter’s disease doesn’t receive the same level of funding for research and public attention as more common disorders because it is so uncommon. Financial assistance and advocacy are essential for hastening the creation of treatments.
People can directly contribute to the fight against Hunter’s disease by supporting groups like the National MPS Society, making donations to research projects, or taking part in clinical trials. Additionally, public awareness is crucial because the more people are aware of this disorder, the quicker diagnoses can be made and more funding for research can be obtained.
The Way Ahead: Why Hunter’s Disease Patients Have Hope
Hunter’s disease patients have a better future than ever before, despite its devastating effects. There is a genuine possibility that scientific developments, especially in the areas of gene therapy and enzyme research, will slow or even stop the progression of disease.
Medical advancements over the next ten years could completely change what it means to have Hunter’s disease. The goal of turning this once incurable illness into a treatable condition might soon come true with sustained research, advocacy, and medical advancement.